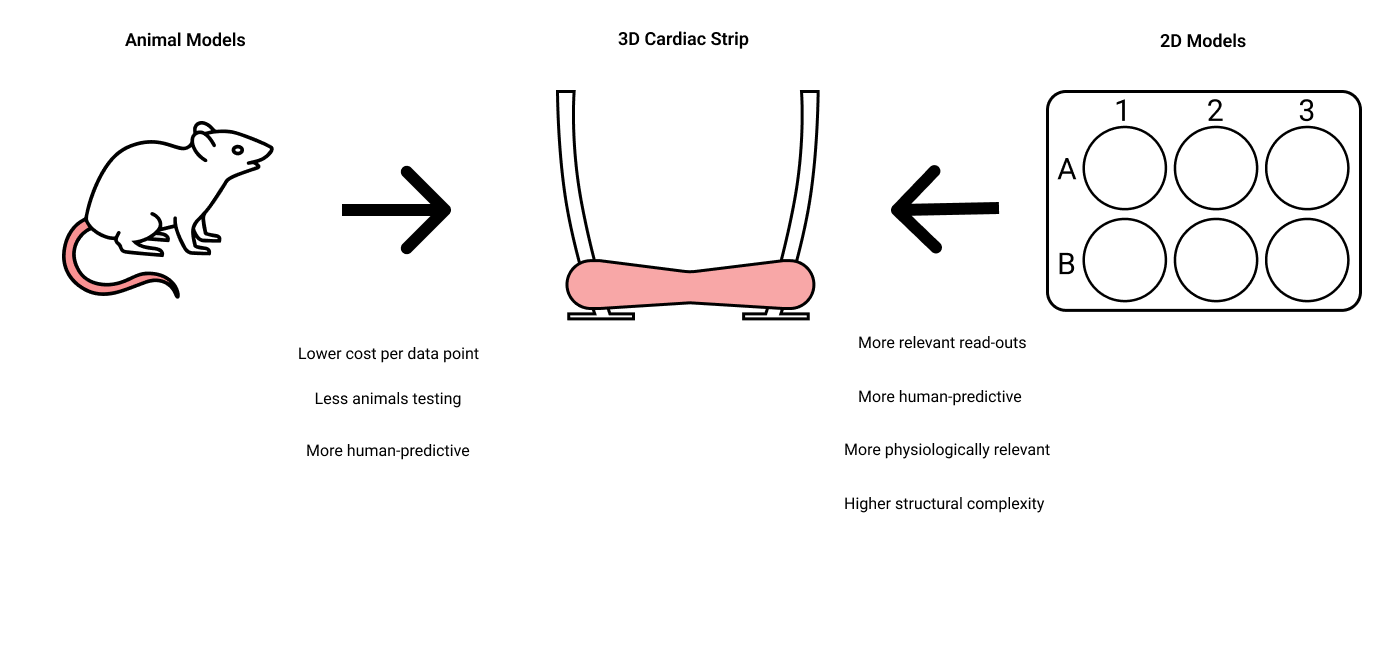
Currently, pre-clinical studies rely mainly on animal models, which have shown over and over again to have an insufficient predictive value for the human heart. The significant differences in genome sequence, protein expression, muscle anatomy and physiology between the rodent and human heart have hampered the development of new drugs for heart failure.
The most commonly used in vitro model for heart disease is a 2D cell culture of cardiomyocytes, which is nothing more than a layer of cardiomyocytes attached to a plastic or glass surface. This culture format has the major disadvantage that plastic and glass are stiff surfaces, thereby completely restraining the natural contractile movement of cardiomyocytes. Since cardiomyocytes in 2D cultures are not able to contract or relax like they do in real human heart tissue, the use of 2D cultures for target validation and discovery for heart failure is limited.
At River BioMedics, we are experts in differentiating human-induced pluripotent stem cells (hiPSCs) into the different cell types which make up the human heart, including cardiomyocytes, cardiac fibroblasts, and cardiac endothelial cells, which can be used to make a human relevant cardiac model. To do this the hiPSC-derived cardiac cells are assembled into a 3D cardiac tissue, in the shape of a strip (therefore also called a “3D Cardiac Strip”). This strip is suspended between two flexible cantilevers to allow for easy measurement of force and relaxation tension.